
Cervical cancer occurs in the cells of the cervix the lower part of the uterus that connects to the vagina. It's a type of cancer that can affect women at any age but often occurs in midlife and is highly treatable when detected early.
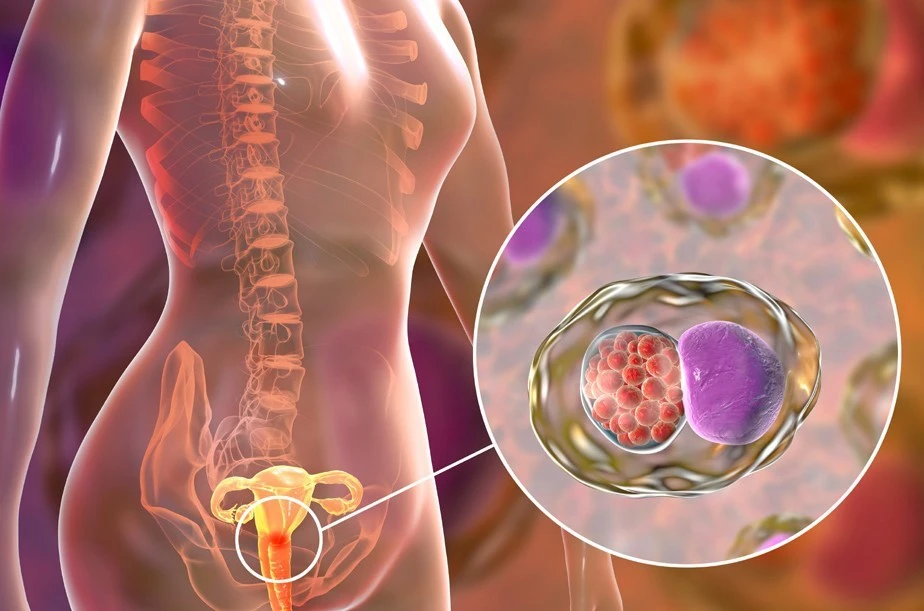
The primary cause of cervical cancer is the Human Papillomavirus (HPV). While many types of HPV exist, only a few cause cancer. Other risk factors include:
In its early stages, cervical cancer may not show symptoms. As it progresses, symptoms might include:
It's important to consult with a healthcare provider if you experience any of these symptoms.
Regular screening tests, such as the Pap smear and the HPV test, can help catch cervical cancer early when it is most treatable. The HPV vaccine is also an effective tool in preventing infections with the cancer-causing types of HPV.
Treatment for cervical cancer depends on several factors, including the stage of the cancer, and may include:
It's crucial to follow a healthcare provider's recommendations and discuss all possible treatment options, including potential side effects.
Remember, regular screenings are the key to early detection and successful treatment of cervical cancer.
Cervical cancer is a type of cancer that occurs in the cells of the cervix the lower part of the uterus that connects to the vagina. Understanding the terminology associated with this condition can empower individuals to better comprehend diagnosis, treatment options, and preventive measures. Below are some commonly used terms in the context of cervical cancer.
HPV is a group of more than 100 viruses, some of which are associated with cervical cancer. High-risk HPV types can cause cervical cell changes that, if untreated, may turn into cancer.
A Pap smear is a screening procedure for cervical cancer. It tests for the presence of precancerous or cancerous cells on the cervix.
When a Pap smear indicates abnormal results, a colposcopy may be necessary. It's a more detailed examination of the cervix using a special microscope called a colposcope to closely inspect the cervical cells.
During or after a colposcopy, a biopsy may be conducted. This involves taking a small sample of tissue from the cervix to be examined more closely in a lab for signs of disease.
CIN grades the severity of abnormal cell changes in the cervix. These changes can be classified as CIN 1 (mild), CIN 2 (moderate), to CIN 3 (severe or carcinoma in situ). Not all CIN turns into cancer, but CIN 3 is treated to prevent potential progression to cervical cancer.
LEEP is a treatment method used to remove abnormal cervical cells. It uses a thin wire loop that carries an electrical current to cut away a thin layer of the cervix's surface, where the abnormal cells are located.
A treatment that uses high-energy rays or particles to destroy cancer cells. Radiation therapy is sometimes used in combination with surgery and chemotherapy to treat more advanced stages of cervical cancer.
Chemotherapy involves the use of drugs to kill cancer cells. It may be administered alone or with radiation therapy for cervical cancer, depending on the stage and characteristics of the cancer.
Understanding these terms can help individuals navigate their cervical cancer journey more effectively, enabling better communication with healthcare providers and a deeper understanding of their treatment options.
Cervical cancer can often go unnoticed until it's in more advanced stages, which makes knowing the warning signs crucial for early detection. Here are the common symptoms and signs associated with cervical cancer:
It's important to remember that these symptoms can also be caused by conditions other than cervical cancer, so consulting a healthcare provider for an accurate diagnosis is crucial. Regular Pap tests can help detect cervical cancer early, often before symptoms appear, making them an essential part of a woman's healthcare routine.
If you experience any of these symptoms, especially if they persist or worsen, it's important to see a healthcare provider. Early detection and treatment can significantly improve the outcome for those with cervical cancer.
Keywords: Cervical Cancer, Symptoms, Abnormal Vaginal Bleeding, Vaginal Discharge, Pelvic Pain, Pain during Urination, Early Detection, Pap tests.
Cervical cancer diagnosis involves a series of steps, aimed at detecting the presence of cancer cells in the cervix. The process usually begins with routine screening tests and might progress to more specific diagnostic tests if initial screenings show abnormalities. Below, we outline the key methods used in diagnosing cervical cancer.
If screening tests indicate abnormalities, further diagnostic tests are conducted to confirm the presence of cervical cancer. These include:
Once the diagnostic tests are completed, if cancer is detected, additional tests will be performed to determine the stage of the cancer. Staging considers the size of the tumor, how deeply the tumor has penetrated, and whether the cancer has spread to nearby lymph nodes or other organs. This information is crucial for developing an effective treatment plan.
Early detection through routine screening is the most effective strategy for preventing and treating cervical cancer. Women are encouraged to have regular screenings and to follow up on any abnormal results with their healthcare provider.

Cervical cancer is a serious health concern worldwide. Early detection plays a crucial role in the successful treatment and management of this disease. Advanced diagnostic tests, including genetic tests, have emerged as vital tools in identifying cervical cancer at its early stages, assessing its progression, and customizing treatment plans. Understanding these tests can empower individuals to make informed decisions about their health.
The Human Papillomavirus (HPV) DNA test is a primary screening tool for cervical cancer. It detects the presence of high-risk HPV types that are known to cause cervical cancer. This test is recommended for women over 30 as part of regular screening or for women of any age who have abnormal Pap test results.
Liquid-based cytology, also known as a liquid Pap test, is a modern alternative to the traditional Pap smear. This test involves collecting cells from the cervix and suspending them in a liquid vial instead of smearing them directly on a microscope slide. It allows for more accurate and comprehensive analysis and can be used alongside HPV DNA testing.
When screening tests suggest abnormalities, a colposcopy may be recommended. This procedure involves using a special microscope called a colposcope to take a closer look at the cervical cells. If suspicious areas are detected, a biopsy, or tissue sample, may be taken for further examination under a microscope to check for cancer cells.
Endocervical Curettage (ECC) is a procedure that scrapes cells from inside the cervical canal. It's often performed alongside a colposcopy if the transformation zone (the area where cervical cells are most likely to become cancerous) cannot be fully visualized.
While there are no genetic tests that directly diagnose cervical cancer, genetic profiling of cancer cells can be incredibly useful. Tests like Next-Generation Sequencing (NGS) can analyze the cancer's genetic makeup, identifying mutations that may influence treatment choices. For example, certain genetic markers can predict the response to targeted therapies, helping personalize treatment approaches.
Advanced imaging tests like Magnetic Resonance Imaging (MRI), Computed Tomography (CT) scans, and Positron Emission Tomography (PET) scans can be used to determine the extent of cervical cancer, including whether it has spread to other parts of the body. These tests are crucial for staging the cancer and planning treatment.
Detecting and understanding cervical cancer involves a combination of advanced diagnostic and genetic tests. These tests offer critical insights into the presence, extent, and molecular characteristics of the disease, guiding more effective and personalized treatment strategies. Regular screening and awareness of these advanced diagnostic options are key to combating cervical cancer effectively.
Cervical cancer, a type of cancer that occurs in the cells of the cervix, is classified into different stages. These stages help doctors determine the extent of the cancer and choose the most effective treatment options. The staging of cervical cancer is primarily based on the FIGO (International Federation of Gynecology and Obstetrics) system.
This early stage, also known as in situ cancer, indicates that cancer cells are present but have not spread beyond the surface layer of the cervix. Treatment at this stage is highly successful.
Stage I cervical cancer signifies that the cancer has grown deeper into the cervix but has not spread to nearby tissues or other parts of the body. It is subdivided based on the size of the tumor and its spread within the cervix:
In stage II, the cancer has spread beyond the uterus and cervix but hasn't reached the pelvic wall or the lower part of the vagina. Like stage I, stage II is further divided:
Stage III cervical cancer indicates further spread, possibly involving the lower third of the vagina or reaching the pelvic wall. It may also cause kidney problems.
The most advanced stage of cervical cancer, stage IV, means the cancer has spread to distant organs.
Understanding the stages of cervical cancer is crucial for selecting the appropriate treatment and predicting outcomes. Regular screening and early detection are essential for effective management of cervical cancer.
Cervical cancer is a type of cancer that occurs in the cells of the cervix. Various strategies can significantly reduce the risk of developing cervical cancer:
In addition to medical precautions, lifestyle choices can also impact cervical cancer risk:
Remember, early detection and prevention are key in the fight against cervical cancer. Regular check-ups and following these preventive measures can help keep your cervical health in check. For more information, consult a healthcare professional.

Cervical cancer treatment depends on the stage of the cancer, the type of cancer, the patient's health and preferences. Typically, treatment includes one or more of the following:
Choosing the best treatment plan involves careful consideration and discussions between the patient and their healthcare team. Each treatment option comes with its risks and benefits, which should be fully understood before proceeding.
It is crucial to follow up with regular check-ups after treatment, as cervical cancer can recur. Additionally, lifestyle changes and support groups can help improve the quality of life during and after treatment.
For more information on cervical cancer treatment, consult with a healthcare provider.
Cervical cancer treatment often involves a combination of therapies, including surgery, radiation therapy, and chemotherapy. The choice of drugs can depend on the cancer's stage, the patient's overall health, and individual treatment goals. Below are some commonly used drugs in the treatment of cervical cancer:
In addition to these, doctors may also prescribe medications to manage symptoms and side effects of the cancer and its treatment, including pain relievers, anti-nausea drugs, and others tailored to the patient's needs.
Patients need to discuss the benefits and risks of these treatments with their healthcare provider to understand the best approach for their specific situation.
Note: This content aims to provide general information on cervical cancer treatment and does not substitute for professional medical advice. Always consult with a healthcare professional for treatment options suitable for you.
Integrative treatment for cervical cancer encompasses a comprehensive approach, combining conventional medical treatments like surgery, chemotherapy, and radiation therapy with complementary therapies. The goal is to not only target the cancer cells but also to enhance the patient's quality of life by managing symptoms and reducing treatment side effects.
The cornerstone of cervical cancer treatment involves traditional medical approaches:
Complementary therapies are used alongside standard medical treatments. These may include:
An integrative treatment plan for cervical cancer offers several benefits:
It is important to discuss any complementary therapies with your healthcare team to ensure they are safe and do not interfere with your primary cancer treatments.
Creating an integrative treatment plan should involve a multidisciplinary team of healthcare professionals, including oncologists, complementary therapy practitioners, nutritionists, and mental health specialists. Together, they can tailor a plan that suits your individual needs, preferences, and treatment goals.
In summary, an integrative approach to cervical cancer treatment combines the best of conventional medical treatments with complementary therapies to treat the disease while enhancing physical and emotional well-being. Open communication with your healthcare team is essential to devising a plan that maximizes the benefits of this holistic approach.

Cervical cancer can be a challenging illness, requiring comprehensive treatment plans that may include surgery, chemotherapy, and radiation. To support health and potentially improve outcomes, many individuals turn to dietary supplements. Here's a look at some commonly used supplements during cervical cancer treatment.
While these supplements may offer benefits, it's crucial to discuss any supplemental usage with your healthcare provider, as certain products could interact with cancer treatments. Tailoring any supplementation to individual needs is key to ensuring safety and effectiveness.
For more information on how to support your health during cervical cancer treatment, consult with healthcare professionals and explore reputable health information sources.
Living with cervical cancer brings unique challenges, but engaging in certain activities can enhance your quality of life during this journey. These activities are designed to support physical health, emotional well-being, and overall recovery. Remember, it's important to consult with your healthcare provider before starting any new activity or exercise regimen.
Walking: A gentle walk outside can boost your mood and improve your cardiovascular health without being too taxing.
Yoga: Specific yoga poses can help stretch and strengthen your body while providing a sense of peace and relaxation.
Meditation: A practice that can help reduce stress and anxiety, improving overall mental health.
Journaling: Writing down your thoughts and feelings can be a therapeutic way to cope with the emotional challenges of cancer treatment.
Cooking healthy meals: Eating a balanced diet is crucial for recovery and maintaining strength. Experiment with recipes that are rich in fruits, vegetables, and lean proteins.
Support groups: Joining a support group can provide a sense of community and understanding from others who are in a similar situation.
Art and craft classes: Engaging in creative activities can be both relaxing and fulfilling, offering a productive outlet for expressing yourself.
Managing cervical cancer is a multi-faceted process that extends beyond medical treatments. Incorporating these recommended activities into your routine can significantly impact your physical and emotional well-being. Always listen to your body and adjust activities based on your energy levels and comfort. Your health and safety should always be the priority.
For more information and tailored advice, please consult your healthcare provider.

Managing cervical cancer involves medical treatment as well as engaging in self-care activities that promote physical and emotional wellness. Here are essential self-care strategies:
Remember, it's important to communicate openly with your healthcare team about your symptoms and how you're feeling. They can offer additional support and adjust your treatment plan as needed to help manage side effects and improve your quality of life.
Contact your healthcare provider for personalized advice before starting any new self-care activities.
Cervical cancer treatment can be a challenging journey, both emotionally and physically. It is crucial to find effective coping strategies that can help alleviate stress, manage side effects, and provide mental comfort during this time. Here we share some ways to cope with cervical cancer treatment that can improve your quality of life.
Begin by gathering information about your specific type of cervical cancer and the treatment options available. Knowing what to expect can reduce anxiety and help you prepare mentally and physically. Discuss with your healthcare team any concerns or questions you have about the procedures, side effects, and the overall treatment plan.
Don't go through this alone. Reach out to support groups or counseling services that specialize in cancer care. Connecting with others who understand your experience can provide comfort and valuable insights. Consider also leaning on friends and family for emotional support and assistance with practical matters like transportation to appointments or meal preparation.
Common side effects of cervical cancer treatment include fatigue, nausea, and pain. Working closely with your healthcare team to manage these side effects is crucial. They can offer medications to alleviate pain and nausea or suggest dietary adjustments to help with recovery. Also, gentle physical activities such as walking or yoga can improve your energy levels and overall well-being.
Maintaining a healthy diet during treatment can help your body stay strong, recover faster, and manage side effects better. Consider consulting a nutritionist who can create a personalized eating plan that accounts for your specific needs and preferences.
Stress reduction is key. Techniques such as meditation, deep breathing exercises, and yoga can help decrease anxiety and improve your emotional health. Even allocating a few minutes a day to these activities can make a significant difference in your stress levels.
Cervical cancer treatment may lead to physical changes in your body. Address these concerns with your healthcare team to receive the appropriate resources, whether it's access to wigs, advice on coping with weight changes, or referral to a physical therapist. Understanding and preparing for these changes can ease the transition and help you maintain a positive self-image.
Each person's journey with cervical cancer is unique, but implementing coping strategies can significantly benefit your treatment experience and quality of life. Remember, it's essential to maintain open communication with your healthcare provider and support network throughout this process. They are there to help you navigate this challenging journey.
This SEO-optimized content focuses on practical tips for individuals undergoing cervical cancer treatment, providing valuable insights on coping mechanisms and strategies to improve well-being.
While the primary treatment for cervical cancer involves medical interventions such as surgery, chemotherapy, or radiation therapy, certain home remedies can support overall health and potentially ease the side effects of conventional treatments. It's crucial to discuss with your healthcare provider before trying any new remedy or supplement to ensure they do not interfere with your medical treatment.
A nutritious diet plays a vital role in supporting your body during cervical cancer treatment. Foods rich in antioxidants, such as fruits and vegetables, can help protect the body's cells. Consider incorporating leafy greens, berries, nuts, and seeds to boost your immune system.
Drinking plenty of water and staying hydrated is essential, especially if you are undergoing chemotherapy or radiation, as these treatments can be dehydrating. Aim for a minimum of eight glasses of water a day, and include hydrating foods like cucumbers and watermelon in your diet.
Gentle exercise, with your doctor's approval, can help maintain physical health, reduce stress, and improve mood. Activities like walking, yoga, or tai chi can be beneficial.
Stress-reduction techniques such as meditation, deep-breathing exercises, and gentle yoga can help manage the emotional and psychological impacts of a cervical cancer diagnosis and treatment.
Some herbal supplements may offer support for your immune system. Popular choices include green tea, ginger, and turmeric for their antioxidant properties. However, it's critical to consult with your healthcare provider before adding any supplements to your routine to avoid potential interactions with treatment.
Maintaining a regular sleep schedule promotes healing and boosts immune function. Aim for 7-9 hours of quality sleep per night and create a relaxing bedtime routine to improve sleep quality.
While these home remedies may support your health, it's important to prioritize the treatment plan outlined by your healthcare team and view these remedies as complementary to, rather than replacements for, conventional treatment.

Being informed is crucial when navigating through your cervical cancer treatment journey. Here are significant questions to discuss with your healthcare team to clarify your treatment path, options, and overall health management.
Discussing these questions with your healthcare team will help you gain a deeper insight into your cervical cancer diagnosis, available treatments, and how to manage your health and well-being during this challenging time.
Remember, being active in your care and decision-making process encourages a partnership with your healthcare team and leads to better treatment outcomes.
The battle against cervical cancer has seen remarkable progress in recent years. With ongoing research and clinical trials, new treatments have emerged, offering hope and improved outcomes for patients. These advancements focus on increasing efficacy, minimizing side effects, and enhancing the quality of life for those affected by this disease.
Immunotherapy has become a beacon of hope in treating various cancers, including cervical. This approach leverages the body's immune system to fight cancer cells more effectively. Pembrolizumab, for instance, is a checkpoint inhibitor that has shown promise in treating advanced cervical cancer by blocking a protein that prevents T cells from attacking cancer cells.
Unlike chemotherapy which affects all rapidly dividing cells, targeted therapy aims at specific genes or proteins that are found in cancer cells or cells related to cancer growth, like blood vessel cells. Tisotumab vedotin is an example of targeted therapy recently approved for recurrent or metastatic cervical cancer. It focuses on tissue factor-expressing tumors, delivering a potent toxin directly to the cancer cells and sparing the healthy ones.
For early-stage cervical cancer, minimally invasive surgical techniques, including laparoscopy and robot-assisted surgery, have revolutionized treatment. These methods result in smaller incisions, reduced pain, fewer complications, and a quicker return to normal activities for patients.
Improvements in radiation therapy provide treatments that are more precise and less harmful to the surrounding healthy tissues. Techniques like intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) allow for higher doses of radiation to be delivered directly to the tumor while minimizing exposure to the adjacent normal tissues, thereby reducing side effects.
As research continues, the future of cervical cancer treatment looks promising. These advancements, alongside the critical role of HPV vaccination in prevention, represent significant strides in the battle against cervical cancer. It's an ever-evolving field, with scientists and doctors relentlessly working towards more innovative and effective treatments.
For anyone facing a cervical cancer diagnosis, it's essential to consult with a healthcare provider to understand the most current and effective treatment options available.
Completing cervical cancer treatment is a significant milestone. However, follow-up care is crucial to monitor recovery, manage side effects, and detect any signs of cancer recurrence. Below are key aspects of post-treatment care for cervical cancer patients.
Patients will need to schedule regular check-ups with their healthcare provider. These visits typically include a physical exam, a pelvic exam, and sometimes a Pap test. The frequency of these appointments varies based on the individual's treatment plan and the doctor's recommendations but often follow a schedule that becomes less frequent over time if no signs of cancer are detected.
Side effects from treatment, such as fatigue, sexual health issues, lymphedema, or menopausal symptoms, may persist or emerge after treatment ends. It's important to communicate with your healthcare team about any ongoing or new symptoms so they can provide appropriate management strategies or therapeutic interventions.
A healthy lifestyle can help support recovery and overall well-being. This may include a balanced diet, regular physical activity, quitting smoking, and limiting alcohol consumption. Additionally, addressing mental and emotional health through counseling or support groups can be beneficial.
Part of follow-up care involves vigilance for signs of cancer recurrence. Patients should report any new symptoms or changes in their health to their doctor immediately. These might include unusual bleeding, pelvic pain, or unexplained weight loss.
Some treatments for cervical cancer may increase the risk of developing a second cancer. Healthcare providers will recommend appropriate screening tests to monitor for other types of cancer as part of the follow-up care plan.
Keeping detailed records of the cancer diagnosis, treatment, and follow-up care plans is important. This information is valuable for ongoing healthcare management and for any new healthcare providers who become part of the patient's medical team.
Frequent communication with your healthcare team, adherence to follow-up appointments, and attention to your overall health and well-being are key components of caring for yourself after cervical cancer treatment.
Being in remission from cervical cancer is a significant milestone. However, maintaining your health is crucial to prevent recurrence. Below are essential tips for care during cervical cancer remission.
Stay vigilant with regular check-ups and screenings. Your healthcare team will schedule follow-up visits, which may include physical exams, Pap tests, and possibly HPV testing. These are critical for catching any changes early.
Eat a balanced diet rich in fruits and vegetables, lean proteins, and whole grains. Regular physical activity can also help you stay healthy and manage stress. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week, as recommended by health guidelines.
It's common to experience a range of emotions during remission. Support groups, therapy, and counseling can be beneficial. Don't hesitate to seek assistance from mental health professionals or support groups. Mindfulness and stress-reduction techniques like meditation and yoga can also support emotional well-being.
If you smoke, seek help to quit, as smoking can increase the risk of cervical cancer recurrence. Limit your alcohol intake as well, following guidelines for moderate consumption.
Talk to your doctor about the human papillomavirus (HPV) vaccine. If you haven't received it yet, it might still be beneficial. The HPV vaccine can prevent infection with certain types of HPV, including some that cause cervical cancer.
Some treatments for cervical cancer can make your skin more sensitive to the sun. Protect your skin with sunscreen, and choose clothing that covers your skin when outdoors.
Being proactive about your health during remission is essential. Listen to your body, and communicate openly with your healthcare team about any concerns. This collaborative approach can help manage your health effectively post-cervical cancer treatment.
For more detailed information and personalized advice, always consult with your healthcare provider.
Cervical cancer is a type of cancer that occurs in the cells of the cervix. Here are some commonly asked questions and answers to help you understand more about cervical cancer.
Most cervical cancer cases are caused by the human papillomavirus (HPV), which is sexually transmitted. Not all strains of HPV cause cervical cancer, but certain types increase the risk.
In the early stages, cervical cancer may cause no symptoms. Advanced cervical cancer may cause abnormal vaginal bleeding or discharge, pain during sex, or pelvic pain.
Getting vaccinated against HPV, undergoing regular screening tests (Pap test or HPV test), practicing safe sex, and avoiding smoking can lower your risk.
The Pap test and the HPV test are two primary screening methods for detecting cervical changes that may indicate cancer or pre-cancer conditions.
Screening should start at age 21. Women aged 21 to 29 should have a Pap test every 3 years. Women aged 30 to 65 should have a Pap test and an HPV test (co-testing) every 5 years or a Pap test alone every 3 years.
While not all cervical cancers can be prevented, vaccination against HPV and regular screening tests can significantly lower the risk of developing cervical cancer.
If diagnosed early, cervical cancer can often be cured. Treatment options vary based on the stage of the cancer and may include surgery, radiation therapy, chemotherapy, or a combination.
Understanding cervical cancer is the first step in prevention. If you have more questions, consider speaking with a healthcare provider for personalized information.