Primary Cutaneous Lymphoma
Published on 27 Feb 2024

What is Primary Cutaneous Lymphoma?
Primary Cutaneous Lymphoma refers to a group of lymphomas that start in the skin. Unlike other types of lymphoma that can spread to the skin, these start primarily within the skin cells themselves. They are a rare form of non-Hodgkin lymphoma.
Types of Primary Cutaneous Lymphoma
There are several types of Primary Cutaneous Lymphoma, but the most common are:
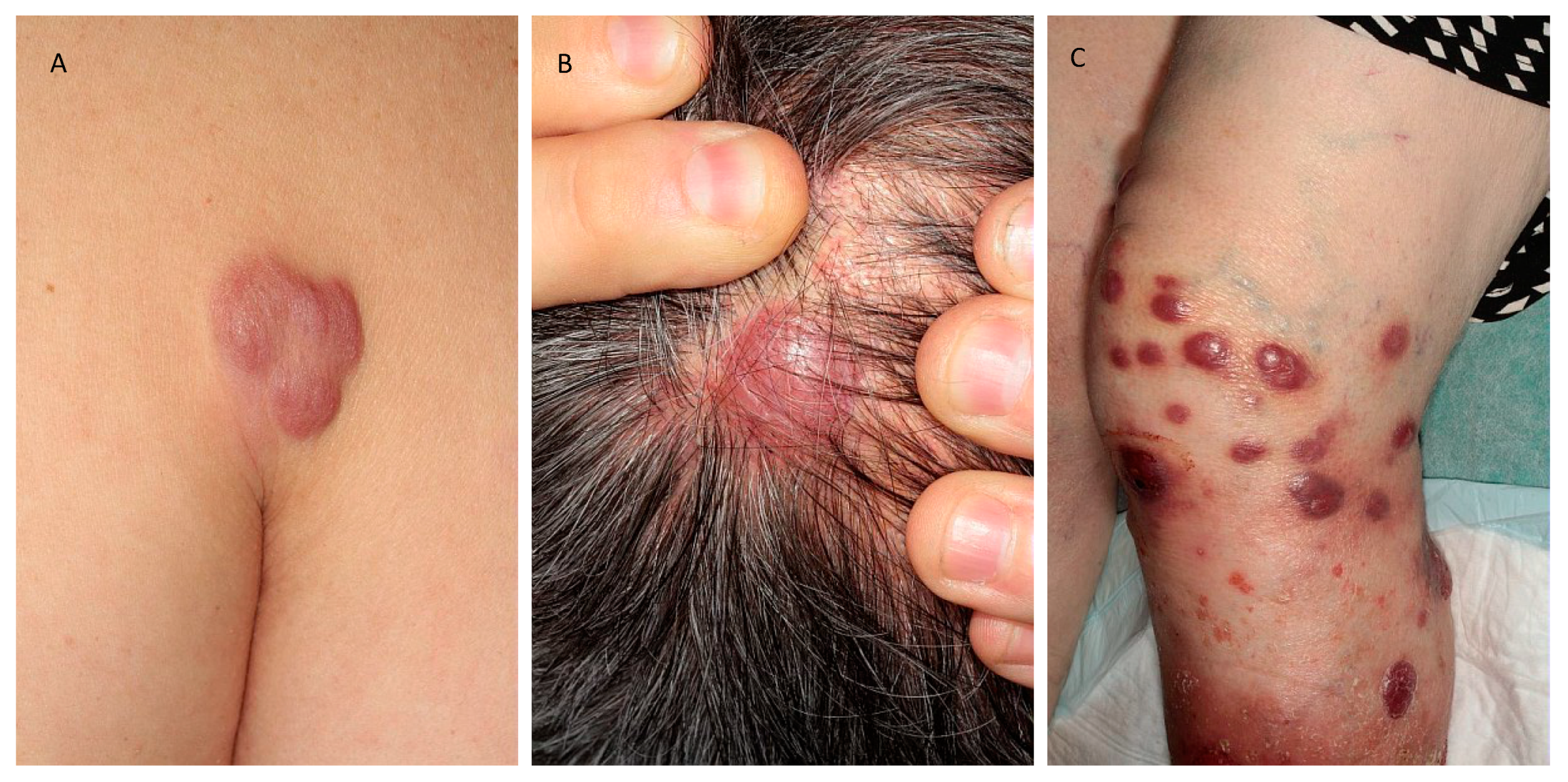
- Mycosis Fungoides: The most prevalent form, characterized by patches, plaques, and tumors on the skin.
- Primary Cutaneous ALCL (Anaplastic Large Cell Lymphoma): It often presents as nodules or tumors that may be ulcerated or not, and is less common than Mycosis Fungoides.
Symptoms
Symptoms can vary but often include:
- Red patches on the skin, often mistaken for eczema or psoriasis
- Tumors that form nodules and may ulcerate
- Itching, which can be severe
- Scaling lesions
Treatment Options
Treatment hinges on the type and stage of the lymphoma but may include:
- Topical treatments such as corticosteroids or chemotherapeutic agents
- Light therapy, including ultraviolet A (PUVA) or B (UVB)
- Systemic treatments for more advanced stages, such as chemotherapy or biologic therapies
It's crucial to consult with a healthcare provider for an accurate diagnosis and tailored treatment plan, as the management of this condition is highly personalized.
For more information on skin health and lymphoma, please consult your healthcare provider.
Understanding Key Terms in Primary Cutaneous Lymphoma
Primary cutaneous lymphoma is a type of cancer that begins in the skin (cutaneous) and is not initially present in the blood or internal organs at the time of diagnosis. This condition is a subset of non-Hodgkin lymphoma and can present in various forms, making it crucial to understand the terminology associated with it. Here, we'll explain some commonly used terms to help you navigate through the information about primary cutaneous lymphoma effectively.
Cutaneous T-cell lymphoma (CTCL)
This is the most common type of primary cutaneous lymphoma, which originates from T-cells, a type of lymphocyte involved in the body's immune response. Mycosis fungoides and Szary syndrome are the most common types of CTCL.
Cutaneous B-cell lymphoma (CBCL)
CBCL arises from B-cells, another type of lymphocyte responsible for producing antibodies. Although less common than CTCL, CBCL typically presents a better prognosis and can manifest in forms like primary cutaneous follicle center lymphoma and primary cutaneous marginal zone lymphoma.
Mycosis Fungoides
A type of CTCL, mycosis fungoides often starts as a rash and can progress over years or even decades to more advanced stages, where tumors may form on the skin.
Szary Syndrome
Another form of CTCL, Szary syndrome is characterized by the presence of cancerous T-cells in the blood, causing widespread redness of the skin and severe itching. Unlike mycosis fungoides, it is generally more aggressive and requires systemic treatment.
Lymphoma
This term refers to a group of blood cancers that develop in the lymphatic system. The primary function of the lymphatic system, part of the immune system, is to fight infections and diseases. Lymphoma affects the lymphocytes (T-cells and B-cells), causing them to behave abnormally.
Skin Biopsy
A critical diagnostic tool for primary cutaneous lymphoma, a skin biopsy involves removing a small piece of skin tissue for examination under a microscope by a pathologist. This helps in confirming the presence and type of lymphoma.
Phototherapy
A treatment option that uses ultraviolet light to treat lesions on the skin's surface. It's often used in early-stage mycosis fungoides.
Topical Treatments
These treatments are applied directly to the skin and include corticosteroids, chemotherapy, and retinoids. They are commonly used for early-stage primary cutaneous lymphoma.
Systemic Therapies
For more advanced stages of primary cutaneous lymphoma, treatments that affect the entire body may be necessary. These include biological therapies that target specific aspects of the immune system, chemotherapy, and extracorporeal photopheresis.
Understanding these terms is key to navigating the complex information surrounding primary cutaneous lymphoma. Whether you're a patient, caregiver, or someone looking to understand more about this condition, grasping this vocabulary will help demystify the disease and its management.
Symptoms and Signs of Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma refers to a group of lymphomas that first appear on the skin. Recognizing the symptoms and signs early can lead to a more effective treatment plan. Below are the most common symptoms and signs associated with Primary Cutaneous Lymphoma.
- Patches or plaques on the skin: One of the most visible signs is the appearance of red or purple patches or plaques. These are typically scaly and may be itchy or even painless.
- Skin lumps: The development of larger, raised nodules or tumors on the skin, which may be of a different colour than the surrounding skin, is another sign. These lumps can sometimes ulcerate (break open) and become infected.
- Skin dryness and eczema-like conditions: Areas of the skin may become exceptionally dry, resembling eczema or dermatitis. This may include peeling or flakiness.
- Changes in pre-existing moles: While not as common, changes in the size, shape, colour, or texture of moles can occur, which necessitates immediate medical examination.
It is important to note that these symptoms can also be related to other benign skin conditions. However, persistent or worsening symptoms warrant a professional medical evaluation. Early detection of Primary Cutaneous Lymphoma significantly improves the effectiveness of the treatment and the patient's quality of life.
For individuals experiencing any of the above symptoms, consulting with a dermatologist or healthcare provider is crucial. They can provide a proper diagnosis through skin biopsies or other relevant tests and recommend the appropriate course of treatment.
Diagnosing Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma (PCL) is a unique form of lymphoma that originates directly in the skin without initial involvement of other organs. Diagnosing this disease involves several steps aimed at confirming the presence and specific type of lymphoma. Due to the complexity of PCL, a comprehensive approach is adopted, involving clinical evaluation, skin biopsies, imaging studies, and laboratory tests to ensure an accurate diagnosis.
Clinical Evaluation
The first step in diagnosing PCL is a thorough clinical evaluation. This involves a detailed medical history and physical examination, focusing on any skin lesions. The appearance, size, and distribution of skin lesions can provide valuable clues. Patients are also asked about symptoms such as itching, pain, or any systemic symptoms like fever or weight loss.
Skin Biopsy
A skin biopsy is one of the most crucial steps in diagnosing PCL. A small sample of the affected skin is removed and examined under a microscope. This allows the pathologist to observe the characteristics of the cells, helping to identify the type of lymphoma. Special stains and immunohistochemistry can be applied to the biopsy sample to detect specific markers on the cells, further aiding in the diagnosis.
Blood Tests
Blood tests may be conducted to assess the general health of the patient and to rule out other conditions. Specific tests can also check for markers indicative of lymphoma or related diseases. These tests can include a complete blood count (CBC), lactate dehydrogenase (LDH) levels, and others as deemed necessary by the physician.
Imaging Studies
Although PCL originates in the skin, imaging studies such as computerized tomography (CT) scans, magnetic resonance imaging (MRI), or positron emission tomography (PET) scans might be recommended to rule out involvement of internal organs or lymph nodes. These imaging techniques help to provide a detailed picture of the body's interior, aiding in the assessment of disease spread.
Molecular and Genetic Tests
In some cases, molecular or genetic tests may be performed on the biopsy sample to identify genetic mutations or specific characteristics of the cancer cells. These tests can provide insights into the prognosis and potential response to treatment.
To conclude, diagnosing Primary Cutaneous Lymphoma involves a multidisciplinary approach where dermatologists, pathologists, and oncologists collaborate to ensure a thorough and accurate diagnosis. This process is crucial for devising an effective treatment plan tailored to the individual patient's condition.
Advanced Diagnostic Tests for Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma (PCL) represents a group of lymphoproliferative disorders that occur in the skin, requiring a meticulous diagnostic approach due to their clinical and histological diversity. Advanced diagnostic tests, including genetic evaluations, play a critical role in ensuring accurate diagnosis and guiding treatment. Here, we explain the key diagnostic tests for PCL, focusing on the latest advancements and genetic assessments.
Skin Biopsy
A skin biopsy remains the first step in diagnosing PCL, where a small skin sample is examined under a microscope. Special stains and immunohistochemistry techniques are employed to detect specific markers that help identify the type of lymphoma.
Immunophenotyping
Immunophenotyping, involving flow cytometry or immunohistochemistry, assesses the expression of surface markers on cells from biopsy samples. This test is crucial for characterizing the lymphoma and differentiating between various subtypes of PCL.
Molecular Genetic Tests
Advances in molecular genetics have significantly improved PCL diagnostics. These tests analyze genetic material (DNA/RNA) from the tumor to identify genetic abnormalities specific to lymphoma cells, such as gene rearrangements or mutations. Key molecular tests include:
- T-cell receptor (TCR) gene rearrangement: Detects clonal T-cell populations, commonly associated with T-cell lymphomas.
- B-cell receptor (BCR) gene rearrangement: Identifies clonal B-cell populations, aiding in the diagnosis of B-cell lymphomas.
- Next-Generation Sequencing (NGS): Provides comprehensive genomic profiling, revealing mutations, gene amplifications, or deletions that can influence prognosis and treatment decisions.
Fluorescence In Situ Hybridization (FISH)
Fluorescence In Situ Hybridization (FISH) detects specific DNA sequences in chromosomes, helping identify genetic abnormalities associated with certain types of PCL. This technique can pinpoint translocations or gene rearrangements that are indicative of specific lymphoma subtypes.
Photographic Documentation
While not a diagnostic test per se, photographic documentation of the skin lesions over time is valuable. It assists in monitoring disease progression and response to treatment.
Conclusion
Accurate diagnosis of Primary Cutaneous Lymphoma relies on a combination of advanced diagnostic tests, including genetic assessments. These evaluations not only confirm the presence of PCL but also guide the choice of treatment, with the potential to improve outcomes for patients. Ongoing research and development in diagnostics are expected to further refine our understanding and management of PCL.
Note: The decision on which diagnostic tests are appropriate should be made in consultation with a healthcare provider, considering the latest guidelines and each patient's specific situation.
Understanding the Stages of Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma (PCL) refers to a group of lymphomas that first appear on the skin before affecting other parts of the body. Knowing the stages of PCL is crucial for determining the most effective treatment and understanding the prognosis. The staging of PCL is generally based on the extent and type of skin involvement, and the presence of disease in lymph nodes, blood, or internal organs.
Stage I
- Stage IA: Less than 10% of the skin surface is covered with patches, plaques, or tumors. There's no evidence of disease in lymph nodes or internal organs.
- Stage IB: More than 10% of the skin surface is involved, but there's still no spread to lymph nodes or internal organs.
Stage II
- Stage IIA: Any amount of skin involvement with patches, plaques, or tumors, but with lymph nodes that are enlarged yet histologically normal.
- Stage IIB: One or more tumors (more than 1cm in diameter) with or without enlarged lymph nodes; no spread to internal organs is detected.
Stage III
- Stage III is characterized by erythroderma, which involves nearly all the skin surface exhibiting redness and peeling. This stage may be associated with abnormal lymph nodes but without the involvement of internal organs.
Stage IV
- Stage IVA: This stage is divided into two parts:
- IVA1: Significant skin involvement along with cancer cells present in the blood (Sezary cells).
- IVA2: Skin involvement with the spread of the disease to lymph nodes (which appear abnormal upon microscopic examination).
- Stage IVB: Any level of skin involvement with the spread of the disease to internal organs, with or without the involvement of lymph nodes or blood.
Each stage of Primary Cutaneous Lymphoma presents unique challenges and treatment options. Early stages often focus on skin-directed therapies, while later stages may require systemic treatment. It's vital to have an accurate diagnosis and stage assessment to tailor the treatment approach effectively for the best possible outcome.
Preventing Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma (PCL) refers to a group of lymphomas that occur directly on the skin, without initially affecting other parts of the body. While the exact cause of PCL is often unknown, making prevention challenging, several strategies might help reduce the risk. Note, however, that these strategies are general and not a guarantee against the disease.
Maintain a Healthy Immune System: A strong immune system can help fight off diseases, including potential cancers. Maintaining a healthy lifestyle through a balanced diet, regular exercise, and adequate sleep can support immune function.
Avoid Excessive Sun Exposure: While sunlight is beneficial for health in moderate amounts, overexposure can damage the skin and potentially increase the risk of skin cancers, including some types of cutaneous lymphoma. Use sunscreen, wear protective clothing, and seek shade during the peak sun hours.
Limit Exposure to Chemicals: Some chemicals, including certain types of pesticides and solvents, might increase the risk of developing lymphoma. Use protective gear when handling chemicals, and follow safety instructions.
Regular Check-Ups: Regular medical check-ups, including skin examinations, can help detect unusual skin changes or conditions early on. Early detection greatly increases the effectiveness of treatment.
Know Your Family History: While PCL is not known to be strongly linked to genetics, knowing your family's health history can provide important context for your own health decisions and vigilance.
It's important to consult with a healthcare professional for personal advice and to discuss any concerns you might have related to skin health and the risk of Primary Cutaneous Lymphoma. While prevention may not always be possible, adopting these healthy habits can contribute to overall well-being and potentially reduce the risk of various types of diseases.
Treatment Options for Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma is a type of non-Hodgkin lymphoma that affects the skin. It's a rare condition that requires specialized care. Treatment options vary depending on the type, severity, and stage of the disease. The goal is to control the spread of cancer, alleviate symptoms, and maintain the quality of life. Here, we explore the common treatment approaches for managing this condition.
Topical Treatments
For early-stage cutaneous lymphoma, topical treatments can be effective. These include:
- Corticosteroids: Applied directly to the skin to reduce inflammation and kill cancer cells.
- Chemotherapy creams: Mechlorethamine gel is an example that targets cancer cells on the skin surface.
- Retinoids: These vitamin A derivatives help slow cancer cell growth.
Phototherapy
Phototherapy, also known as light therapy, involves exposing the skin to ultraviolet (UV) light. UVA or UVB light can target and destroy cancer cells. Sometimes, medications are used in combination with UV light to make cancer cells more sensitive to treatment, known as PUVA therapy.
Radiation Therapy
Localized radiation therapy targets specific areas of the skin affected by lymphoma, preserving surrounding healthy tissue. This approach can be particularly effective for tumors that are resistant to other forms of treatment.
Systemic Treatments
Advanced stages of cutaneous lymphoma might require systemic treatments, which affect the entire body:
- Chemotherapy: Drugs are used to kill cancer cells or stop them from growing.
- Biologic Therapy: Also called immunotherapy, these treatments boost or manipulate the immune system to fight cancer.
- Targeted Therapy: Drugs or other substances target and attack specific cancer cells with minimal harm to normal cells.
Stem Cell Transplant
In some cases, a stem cell transplant may be an option, especially for aggressive types of cutaneous lymphoma. This procedure involves replacing diseased bone marrow with healthy stem cells.
The choice of treatment depends on various factors, including the specific type and stage of cutaneous lymphoma, as well as the patient's overall health and preferences. Patients need to discuss all available treatment options with their healthcare team to make informed decisions about their care.
Consultation with a Specialist: Managing primary cutaneous lymphoma often requires a multidisciplinary approach. Patients should consult dermatologists, oncologists, and other specialists experienced in treating skin lymphomas to ensure the most effective treatment plan.
Note: This content is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition.
Treatment Options for Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma (PCL) is a type of non-Hodgkin lymphoma that affects the skin. It is a rare disease, and its treatment often requires a multi-disciplinary approach. The choice of therapy usually depends on the specific type of cutaneous lymphoma, its stage, and the patient's overall health. Here is an overview of the commonly used treatment options for PCL.
- Topical Treatments: These are applied directly to the skin and are typically used for the early stages of the disease. Examples include:
- Corticosteroids: Powerful anti-inflammatory drugs that can help reduce skin lesions.
- Topical Chemotherapy: Such as mechlorethamine gel, which directly targets cancer cells in the skin.
- Topical Retinoids: Analogs of Vitamin A that can slow the growth of skin cells.
- Topical Immunomodulators: Such as imiquimod, which boosts the immune response against cancer cells.
- Phototherapy: Uses ultraviolet light to kill cancer cells in the skin. The two main types are Ultraviolet A (UVA) and Ultraviolet B (UVB).
- Radiation Therapy: Directs high-energy rays at the cancer to kill or shrink the cancer cells. This method is particularly effective for localized or solitary lesions.
- Systemic Treatments: These are drugs that work throughout the body and are used for more advanced stages or when the disease is resistant to topical treatments. They include:
- Chemotherapy: Drugs like methotrexate or doxorubicin can attack rapidly dividing cells, including cancer cells.
- Biologic Therapy: These drugs use the body's immune system to fight cancer. For example, interferons can help slow the growth of cancer cells.
- Targeted Therapy: Drugs that target specific vulnerabilities in cancer cells. Brentuximab vedotin is a targeted therapy used for certain types of cutaneous lymphoma.
- Stem Cell Transplant: This is a more intensive treatment option where the patient's diseased bone marrow is replaced with healthy stem cells.
Choosing the right treatment for Primary Cutaneous Lymphoma requires a careful evaluation of the disease and a personalized treatment plan. Ongoing research into the causes and treatments of PCL is leading to more effective and targeted therapies, offering hope for those affected by this condition.
Integrative Treatment for Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma is a type of cancer that begins in the white blood cells and manifests in the skin. It's a rare condition that requires a multifaceted approach to treatment. Integrative treatment combines traditional medical treatments with complementary therapies to address the disease from all angles, focusing on the patient's overall well-being.
Traditional Treatments
The foundation of treating Primary Cutaneous Lymphoma typically involves traditional treatments such as:
- Topical therapies: Including corticosteroids, chemotherapeutic agents, and retinoids to control symptoms and prevent progression.
- Radiation therapy: Utilizes high-energy rays to target and destroy cancer cells.
- Systemic medications: Such as interferon or methotrexate, are used to treat the entire body and manage more advanced stages.
Complementary Therapies
Complementary therapies aim to improve quality of life and support overall health, including:
- Diet and nutrition: Tailoring dietary choices to support the body's natural defences and manage the side effects of traditional treatments.
- Mind-body practices: Such as yoga and meditation, to reduce stress and improve mental well-being.
- Physical activity: Regular, gentle exercise like walking or swimming to maintain strength and stamina.
Integrating Treatments for Optimal Care
The integration of these treatments involves a personalized approach, tailoring therapies to the individual's specific condition, needs, and preferences. Communication between healthcare providers is crucial to ensure that the combination of treatments offers the highest benefit with the least risk to the patient.
Patients are encouraged to engage actively in their care, discussing options and preferences with their healthcare team. This collaborative approach aims not only to treat cancer but also to enhance the patient's quality of life through supportive care measures.
Conclusion
Integrative treatment for Primary Cutaneous Lymphoma represents a shift from focusing solely on the disease to a more holistic view of the patient's health and well-being. By combining traditional and complementary approaches, patients can receive personalized, comprehensive care that addresses the many facets of living with this condition.
For individuals diagnosed with Primary Cutaneous Lymphoma, consulting with a team of healthcare providers knowledgeable in both traditional oncology and holistic therapies will offer the best strategy for managing the disease and achieving a high quality of life.
Common Supplements for Primary Cutaneous Lymphoma Support
Managing Primary Cutaneous Lymphoma (PCL) often involves medical treatments including chemotherapy and radiation. However, many patients and healthcare providers also consider dietary supplements as part of a comprehensive care plan. These supplements are not a cure but may help support overall health and well-being during treatment. Here are some commonly used supplements:
- Omega-3 Fatty Acids: Found in fish oil, these supplements are known for their anti-inflammatory properties and may help reduce some side effects of cancer treatments.
- Vitamin D: Many individuals with PCL have low levels of Vitamin D. Supplementation can support bone health and may have immune-enhancing effects.
- Curcumin: This compound is extracted from turmeric and is believed to have anti-inflammatory and antioxidant properties. Curcumin may help mitigate some side effects of chemotherapy.
- Green Tea Extract: Rich in antioxidants, green tea extract may support immune health and has been studied for its potential cancer-fighting properties.
- Selenium: This mineral is essential for the proper functioning of the immune system and may help protect against oxidative damage during cancer treatments.
- Probiotics: Maintaining gut health is crucial during cancer treatment. Probiotics can help maintain a healthy gut flora, which is vital for immunity and digestion.
It's important to note that supplements should not replace conventional cancer treatments. Always consult with a healthcare provider before starting any new supplements, especially during cancer treatment, as some supplements may interact with medications or may not be suitable for all individuals.
Maintaining a healthy lifestyle with a balanced diet, regular physical activity, and adequate rest, along with the supervised use of supplements, can support overall health during the treatment of Primary Cutaneous Lymphoma.
Recommended Activities for Primary Cutaneous Lymphoma Patients
Living with Primary Cutaneous Lymphoma (PCL) can be challenging, but engaging in certain activities can help manage the condition and improve quality of life. Here are some recommended activities tailored for individuals with PCL, aiming to promote well-being and comfort:
- Gentle Exercise: Mild exercises such as walking, yoga, and swimming can boost your mood and energy levels without overexerting the skin. Always remember to wear sun-protective clothing if exercising outdoors.
- Skin Care Routine: Developing a gentle skincare routine with products that soothe and hydrate the skin can help manage symptoms. Avoid harsh chemicals and opt for natural, fragrance-free products.
- Stress-Relief Activities: Stress management is crucial for PCL patients. Activities like meditation, deep breathing exercises, and mindfulness can help reduce stress levels, which may, in turn, help in managing symptoms.
- Art and Hobby Groups: Engaging in creative activities such as painting, crafting, or joining hobby groups can serve as a therapeutic outlet and foster a sense of community and support.
- Nutritional Foods: Eating a balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support overall health. Some patients may also benefit from consulting a nutritionist to tailor a diet plan to their specific needs.
- Educational Workshops: Participating in workshops about PCL can empower patients by expanding their knowledge about their condition and exploring new ways to manage it effectively.
PCL patients need to listen to their bodies and adjust activities based on their comfort and energy levels. Consulting with healthcare professionals before starting any new activity is advisable to ensure it is safe and suitable for their specific condition.
By incorporating these activities into their lifestyle, individuals with Primary Cutaneous Lymphoma can foster physical and emotional well-being, paving the way for an improved quality of life.
Effective Self-Care Activities for Primary Cutaneous Lymphoma
Living with Primary Cutaneous Lymphoma (PCL) requires not just medical treatment but also engaging in self-care practices that support overall well-being. Here are some self-care activities that can help manage symptoms and improve quality of life:
- Maintain a Gentle Skin Care Routine: Use mild, fragrance-free soaps and moisturizers to help keep your skin hydrated and reduce irritation. Avoid hot showers or baths, which can strip the skin of its natural oils.
- Protect Your Skin from the Sun: UV exposure can worsen PCL symptoms. Wear protective clothing, seek shade, and apply broad-spectrum sunscreen with a high SPF to protect your skin from sun damage.
- Stay Active: Regular exercise can improve your physical and mental health. Choose low-impact activities that you enjoy, like walking, yoga, or swimming, to keep your body active without overexerting yourself.
- Eat a Balanced Diet: A nutritious diet supports your immune system and overall health. Focus on eating plenty of fruits, vegetables, whole grains, and lean proteins. Consult with a nutritionist to tailor your diet to your specific health needs.
- Manage Stress: Stress can exacerbate PCL symptoms. Practice stress-reduction techniques such as meditation, deep breathing exercises, or mindfulness to help keep stress levels in check.
- Seek Support: Connecting with others who understand what you're going through can be incredibly beneficial. Consider joining a support group for individuals with PCL or similar conditions.
Remember, it's important to discuss any new self-care strategies with your healthcare provider to ensure they're safe and appropriate for your specific condition. By incorporating these self-care activities into your daily routine, you can better manage your Primary Cutaneous Lymphoma symptoms and lead a healthier, more fulfilling life.
Coping Strategies for Primary Cutaneous Lymphoma Treatment
Dealing with a diagnosis of Primary Cutaneous Lymphoma (PCL) can be challenging. However, numerous strategies can help patients cope with the treatment process. It's essential to take both your physical and emotional well-being into account.
Understand Your Treatment Options
Getting to know more about your treatment options can make you feel more in control. Speak to your healthcare provider about the treatments available, potential side effects, and any concerns you might have. This knowledge can help alleviate some of the anxiety associated with the unknown.
Maintain a Support System
Having a strong support system in place can make a significant difference in coping with PCL. This can include family, friends, support groups, or online forums. Sharing your thoughts and experiences with others who understand can be incredibly comforting.
Manage Side Effects
Consult with your healthcare team to find effective ways to manage treatment side effects. This might include dietary changes, medication for symptom relief, or physical therapy. Managing these side effects can help improve your quality of life during treatment.
Focus on Nutrition and Exercise
Maintaining a balanced diet and staying physically active can help support your body through treatment. Nutritious foods can boost your energy levels and immune system, while exercise can reduce fatigue and stress.
Practice Mindfulness and Relaxation Techniques
Stress-reduction techniques such as meditation, deep breathing, and yoga can help you cope with the emotional stress of PCL treatment. These practices can help keep your mind calm and alleviate anxiety.
Stay Informed but Avoid Overload
While staying informed about your condition is important, too much information can be overwhelming. Limit your research to reputable sources and don't hesitate to discuss any information you find with your healthcare provider.
Set Realistic Goals
Setting achievable goals can give you a sense of purpose and something to look forward to. These goals can be related to your treatment, personal hobbies, or spending time with loved ones.
Seek Professional Help if Needed
It's crucial to recognize when you might need professional help. If you're struggling with anxiety, depression, or coping in general, consult a mental health professional. Emotional and psychological support is as important as physical treatment in your healing journey.
Dealing with Primary Cutaneous Lymphoma can undoubtedly be tough, but employing coping strategies can make the treatment journey more manageable. Remember, you're not alone, and support is always available.
Home Remedies for Primary Cutaneous Lymphoma
Dealing with Primary Cutaneous Lymphoma (PCL) can be challenging, but incorporating certain home remedies alongside your medical treatment may help manage symptoms and improve your quality of life. It's essential to consult your healthcare provider before trying any new remedy to ensure it's safe for your specific condition.
Moisturize Your Skin
Keeping your skin moisturized is crucial. Dry skin can be more susceptible to irritation and infection, which people with PCL should avoid. Use hypoallergenic and fragrance-free moisturizers to keep your skin hydrated.
Mild Skin Care Products
Opt for mild, gentle skin care products. Harsh soaps, lotions, and chemicals can irritate the skin. Choose products specifically designed for sensitive skin to help minimize reactions.
Healthy Diet
Eating a well-balanced diet can support your immune system and overall health. Focus on incorporating a variety of fruits, vegetables, whole grains, and lean proteins into your meals. Foods rich in antioxidants may particularly benefit the skin.
Stay Hydrated
Drinking plenty of water is essential for maintaining healthy skin. Aim for at least 8 glasses of water a day to help keep your skin hydrated from the inside out.
Avoid Sun Exposure
Protecting your skin from the sun is crucial as sunlight can exacerbate PCL symptoms. Wear protective clothing, use sunscreen with a high SPF, and avoid the sun during peak hours to minimize your exposure.
Gentle Exercise
Engaging in gentle, low-impact exercise can improve circulation, support your immune system, and enhance your overall well-being. Consult with your healthcare provider to determine the best exercise routine for your condition.
Stress Management
Managing stress is important for individuals with PCL. Stress can impact your immune system and exacerbate symptoms. Consider practices like meditation, yoga, or deep-breathing exercises to help manage stress levels.
While these home remedies can offer support and relief, they should not replace the treatment plan prescribed by your healthcare provider. Always discuss any new remedies or changes to your care plan with a medical professional.
Key Questions to Ask Your Healthcare Team About Primary Cutaneous Lymphoma Treatment
Being diagnosed with Primary Cutaneous Lymphoma can be challenging, and understanding the best course of action requires a collaborative approach with your healthcare team. Here are essential questions to discuss to ensure you have a comprehensive understanding of your treatment plan.
- What type of Primary Cutaneous Lymphoma do I have?
This information is crucial as it directly influences your treatment options and prognosis. - What stage is my cutaneous lymphoma?
Knowing the stage helps in determining the severity and spread of the disease, which is vital for planning treatment. - What treatment options are available?
Different treatments may be suggested based on your type and stage of lymphoma. It's important to know all available options, including the latest treatments and clinical trials. - What are the expected benefits and possible side effects of each treatment?
Understanding the potential outcomes and risks of each treatment can help you make an informed decision. - How will the treatment be administered, and how long will it last?
This information will help you prepare for the treatment process and any adjustments you need to make in your daily life. - How is treatment effectiveness monitored?
Learn how and when your response to treatment will be evaluated, including the types of tests and monitoring frequency. - What supportive care or symptom management resources are available?
Managing symptoms and side effects is crucial for maintaining your quality of life during treatment. - How might treatment affect my daily life?
Knowing the impact on your daily routines can help you plan and make any necessary adjustments. - Are there any lifestyle changes I should make to support my treatment or general health?
Dietary changes, physical activity, and other lifestyle adjustments can sometimes help support your health and well-being during treatment. - What is the cost of treatment, and is it covered by my insurance?
Understanding the financial aspects of your treatment is essential for planning and avoiding surprises.
It's also beneficial to ask for patient resources, support groups, or counselling services that could help you and your family navigate the emotional and practical challenges of living with Primary Cutaneous Lymphoma.
Remember, your healthcare team is there to support you through your treatment journey. Don't hesitate to ask any questions or express concerns you might have about your treatment plan.
Advancements in Primary Cutaneous Lymphoma (PCL) Treatments
The landscape of Primary Cutaneous Lymphoma (PCL) treatment has witnessed significant advances, offering new hope and improved outcomes for patients. PCL, a rare form of non-Hodgkin lymphoma that appears on the skin, has seen progress in both targeted therapies and immunotherapies. Keeping abreast of these developments is crucial for patients and healthcare providers alike.
Targeted Therapies
One of the forefronts in PCL treatment is the advent of targeted therapies. These treatments focus on specific cellular mechanisms or proteins involved in the growth and spread of cancer cells, sparing the healthy cells and reducing side effects. For instance, Brentuximab vedotin, an antibody-drug conjugate, has shown efficacy in treating CD30+ PCL, marking a significant step forward.
Immunotherapies
Immunotherapies have revolutionized PCL treatment by bolstering the body's immune system to fight cancer. Drugs like checkpoint inhibitors have been explored in clinical trials, with promising outcomes in providing durable responses in some PCL patients. These treatments can reactivate the immune system to identify and destroy cancer cells effectively.
Phototherapy and Radiation
Advancements in phototherapy and radiation therapy techniques continue to play pivotal roles in PCL management, particularly for early-stage or localized disease. Refined phototherapy methods, such as narrow-band ultraviolet B (NB-UVB), offer targeted and less harmful options. Furthermore, low-dose radiation therapy has been optimized for effectiveness and minimized side effects.
Emerging Therapies
Research into new treatments, including small molecule inhibitors and gene therapies, is ongoing. These emerging therapies hold the promise of more personalized and precise treatment options for PCL patients in the future.
In conclusion, the landscape of Primary Cutaneous Lymphoma treatment is rapidly evolving, with targeted therapies, immunotherapies, and advanced radiation techniques leading the way. As research continues, the hope for more effective and less toxic treatments grows, offering new opportunities for patient care and management.
For individuals facing PCL, staying informed about the latest treatment options is essential. Consultation with a healthcare provider specializing in dermatology or oncology can provide guidance tailored to individual cases and access to the most current and effective therapies.
Follow-up care for Primary Cutaneous Lymphoma
After completing treatment for Primary Cutaneous Lymphoma (PCL), ongoing follow-up care is crucial. This not only helps in detecting any signs of the disease returning but also manages any potential side effects from the treatment. Here's a brief guide on the necessary follow-up care for PCL survivors.
- Regular Check-Ups: Schedule regular visits with your oncologist. These check-ups usually involve physical exams, blood tests, and possibly imaging tests, to look for signs of lymphoma or any other health issues.
- Skin Self-Exams: Since PCL affects the skin directly, performing regular self-exams is vital. Be attentive to changes in the size, colour, or feel of skin lesions and report these to your doctor.
- Management of Side Effects: Some treatments for PCL can lead to side effects that may last after treatment ends. Work with your healthcare team to manage any ongoing or new side effects.
- Emotional and Psychological Support: Recovering from lymphoma can be challenging, not just physically but also emotionally. Consider seeking support from cancer support groups, a counsellor, or psychologists specialized in helping cancer survivors.
- Maintain a Healthy Lifestyle: Adopting a healthy lifestyle can enhance your well-being. This includes a balanced diet, regular physical activity, adequate sleep, and avoidance of tobacco and excessive alcohol.
Remember, each individual's follow-up care is unique. Your follow-up care plan should be designed to fit your specific needs, based on the type of PCL, treatments you've undergone, and your overall health. Staying informed and engaged with your healthcare team is key to navigating the journey after PCL treatment.
Keywords: Primary Cutaneous Lymphoma, follow-up care, treatment, oncologist, side effects, skin self-exams
Maintaining Health in Primary Cutaneous Lymphoma Remission
Being in remission from Primary Cutaneous Lymphoma is a significant milestone. However, maintaining good health during this period is crucial. Here are some tips to help you stay healthy and potentially prevent recurrence.
- Regular check-ups: Schedule regular visits with your healthcare provider. Early detection of any changes can aid in prompt intervention.
- Sun protection: Exposure to ultraviolet (UV) light can be a risk factor. Wear sunscreen with a high SPF, seek shade, and wear protective clothing when outdoors.
- Healthy diet: Consume a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Certain foods may have cancer-fighting properties.
- Exercise: Engage in regular physical activity. Exercise can improve your mood, boost your energy, and maintain your weight.
- Avoid smoking: Smoking is a risk factor for many cancers, including lymphoma. Seeking help to quit smoking can improve your overall health.
- Limit alcohol intake: Consuming alcohol in moderation is crucial. Excessive alcohol use can weaken your immune system.
- Stress management: Finding ways to manage your stress, such as through meditation, yoga, or hobbies, can improve your mental health.
- Stay informed: Keeping up-to-date with the latest research on Primary Cutaneous Lymphoma can help you make informed decisions about your health care.
Remember, maintaining a healthy lifestyle is key to staying well during remission. While there's no guaranteed way to prevent cancer from returning, these strategies can help support your overall health and well-being. Always consult with your healthcare provider before making significant changes to your health regimen.
For more information on managing Primary Cutaneous Lymphoma, visit [your health organization's website] or speak to your healthcare professional.
Frequently Asked Questions about Primary Cutaneous Lymphoma
Primary Cutaneous Lymphoma (PCL) represents a group of lymphomas that occur on the skin. Here are some common questions and straightforward answers about this condition.
What is Primary Cutaneous Lymphoma?
Primary Cutaneous Lymphoma is a category of non-Hodgkin lymphoma that starts in the skin. Unlike other types of lymphoma that might spread to the skin, PCL originates there. It's characterized by the accumulation of cancerous lymphocytes in the skin, leading to various symptoms, notably skin lesions.
What causes PCL?
The exact cause of Primary Cutaneous Lymphoma remains unknown. However, it's believed to result from changes or mutations in the DNA of lymphocytes, which then grow uncontrollably. Factors such as viral infections, exposure to certain chemicals, and a weakened immune system can increase the risk, though most cases occur without a clear predisposing factor.
What are the symptoms of PCL?
Symptoms often include red, scaly patches or plaques on the skin that might be itchy. In some types of PCL, tumours or raised lesions can develop. The symptoms can vary widely depending on the specific subtype of PCL.
How is PCL diagnosed?
Diagnosis involves a skin biopsy, where a small piece of skin is removed and examined under a microscope. Additional tests such as blood tests, imaging scans, and sometimes lymph node biopsies may be conducted to determine the extent and nature of the disease.
What are the treatment options for PCL?
Treatment varies depending on the type and stage of PCL. Options might include skin-directed therapies such as topical steroids, light therapy (phototherapy), and radiation therapy. In more advanced cases, systemic treatments like chemotherapy, biological therapy, or targeted therapy may be necessary.
Is PCL curable?
The prognosis and potential for cure depend on the specific type of PCL, its stage at diagnosis, and how well the tumour responds to treatment. Early-stage PCLs, especially those confined to the skin, often have a favourable outcome with treatment.
Can PCL spread beyond the skin?
While PCL begins in the skin, it can spread to nearby lymph nodes, blood, or other parts of the body in more advanced stages. Regular monitoring and treatment adjustments are crucial to manage the spread.
How can I support someone with PCL?
Supporting someone with PCL involves offering emotional support, helping them manage their symptoms or treatment side effects, and encouraging them to follow their treatment plan. Educating yourself about the condition can also help in providing meaningful support.
For more detailed information, consult a dermatologist or an oncologist specialized in lymphomas.























