
The Whipple Procedure, medically known as Pancreaticoduodenectomy, is a complex surgical operation primarily executed to treat pancreatic cancer. This procedure might sound daunting at first, but understanding its purpose and implications can shed light on why it's considered a beacon of hope for many facing this difficult diagnosis.
Pancreatic cancer, known for its aggressive nature and challenging prognosis, is not the sole condition treated by the Whipple procedure. It's also applied in the treatment of tumors in the pancreas, bile duct, and duodenum (the first part of the small intestine), as well as certain chronic pancreatitis cases. The versatility of this procedure underscores the critical role it plays in gastrointestinal surgical oncology.
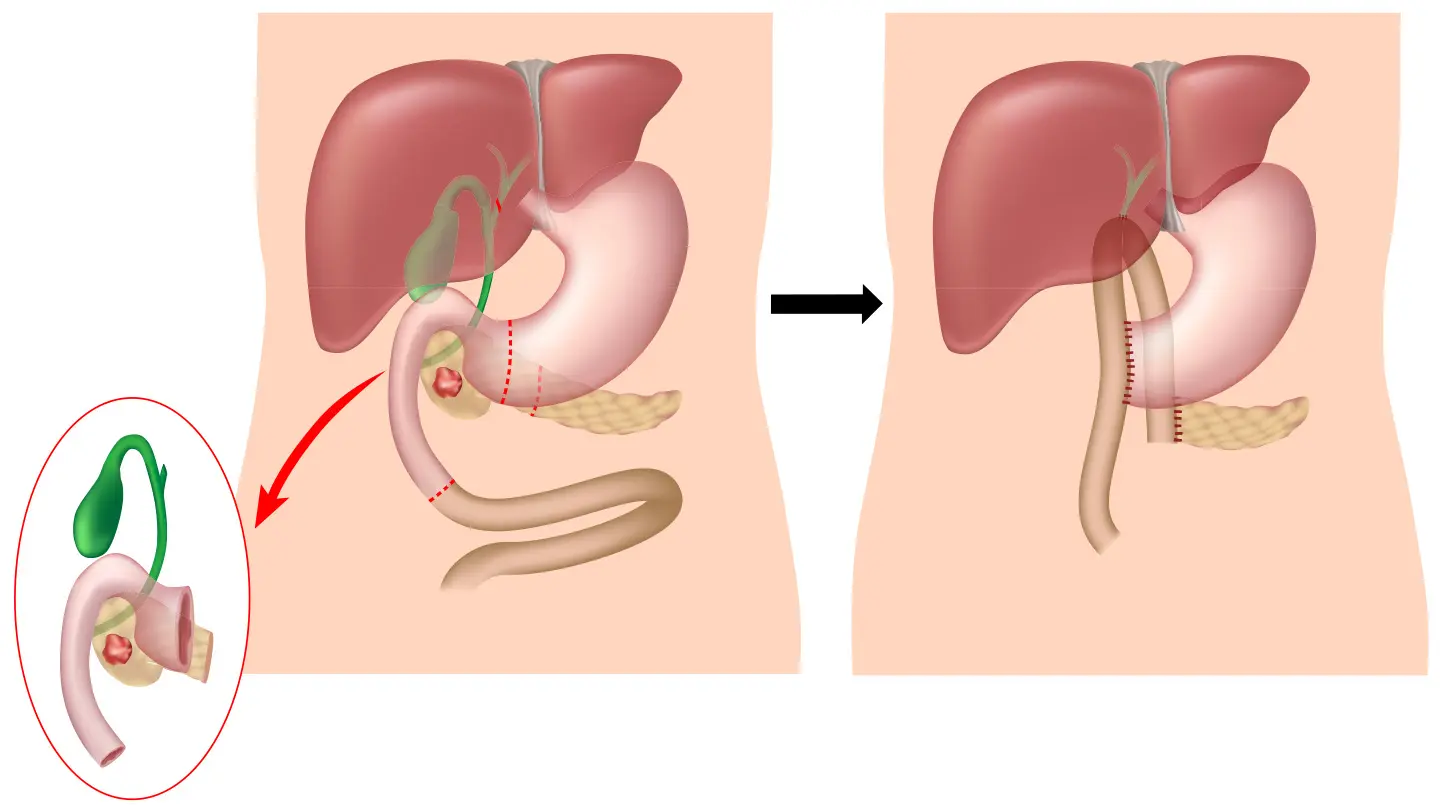
At its core, the objective of the Whipple Procedure is to remove the cancerous tumor and prevent the disease from spreading, thereby increasing the patient's survival rate. The operation involves the removal of the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder, and a portion of the bile duct. A meticulous reconstruction of the digestive system follows to ensure functionality post-operation.
Why might this procedure be necessary? For many patients, the Whipple Procedure represents a vital treatment option that can significantly extend life expectancy. Given the rapid progression and aggressive nature of pancreatic and related cancers, early detection and surgical intervention are crucial. It's precisely for these reasons that the surgery, despite its complexity and association with significant recovery time, is often recommended.
However, it's important to note that not every patient with pancreatic cancer is a candidate for the Whipple Procedure. Various factors, such as the stage of cancer, the overall health of the patient, and the tumor's location, influence the eligibility for this surgery. Consultation with a specialist in gastrointestinal oncology is essential to assess the feasibility and potential benefits of undergoing this procedure.
Nutrition plays a crucial role in recovery and overall well-being during cancer treatment. Post-surgery, patients may need to adapt their diets significantly. Including nutrient-rich vegetarian meals can aid in the recovery process, providing essential vitamins, minerals, and fibers necessary for healing and strength. Foods like lentils, beans, quinoa, and plenty of fresh vegetables and fruits should take precedence to support the body's healing process.
Understanding the Whipple Procedure is the first step for patients and their families in navigating the complexities of pancreatic and related cancers. Although the journey may be challenging, advancements in medical science and surgical techniques continue to provide hope and improve outcomes for those affected by these conditions.
If you or a loved one is gearing up for a Whipple procedure to tackle pancreas, gallbladder, or duodenal cancer, preparation is key. This surgery, being complex, requires thorough planning for a successful outcome. In this section, we'll delve into vital steps patients need to take before undergoing surgery, highlighting dietary restrictions, pre-operative tests, and mental health considerations. Remember, a personalized preparation plan is essential for the best results.
Before undergoing the Whipple procedure, your diet might need adjustments. It's paramount to maintain a nutrient-rich diet that supports healing and energy levels. Fruits, vegetables, whole grains, and legumes can be powerhouses of vitamins and minerals necessary for recovery. However, you might need to follow specific dietary instructions from your healthcare team. These could include fasting or consuming only clear liquids a day before the surgery. Always consult with a nutritionist to tailor the diet to your needs.
Preparation for the Whipple procedure involves several pre-operative tests to ensure you're a suitable candidate. These can include blood tests, imaging studies like MRI or CT scans, and perhaps cardiac evaluation to assess your heart's health. These tests provide a detailed picture of your condition, helping surgeons plan the procedure with precision.
Undergoing major surgery can be daunting, and it's normal to experience a range of emotions. Engaging in discussions with a mental health professional can be incredibly beneficial. They can offer strategies to cope with anxiety, stress, and any fears you might have about the surgery or the recovery process. Support groups and therapy sessions can also be valuable resources for both patients and their families.
In summary, preparing for the Whipple procedure demands attention to various aspects of your health. By focusing on dietary adjustments, completing necessary pre-operative tests, and taking care of your mental health, you're laying the groundwork for a smoother surgery and recovery. Always communicate closely with your healthcare team to develop a preparation plan that's tailored specifically to you.
The Whipple procedure, also known as pancreaticoduodenectomy, is a complex surgery aimed at treating cancer, particularly when it's located in the pancreas head. This procedure can be daunting to understand, so let's break down the process, including the surgical approaches, organs involved, and required expertise.
Open Surgery vs. Minimally Invasive Techniques: Initially, the Whipple procedure was exclusively performed as open surgery, requiring a large incision in the abdomen. However, with the advancement in surgical techniques, minimally invasive options, such as laparoscopic and robotic surgery, have become available. These approaches involve smaller incisions, potentially leading to shorter recovery times and less post-operative pain for the patient.
In the Whipple procedure, the surgeon removes the head of the pancreas, the duodenum (the first part of the small intestine), the gallbladder, and part of the bile duct. Depending on the patient's condition, a portion of the stomach may also be removed. Following the resection, the remaining organs are reconstructed to enable digestion. This involves attaching the remaining pancreas to the small intestine, so digestive enzymes and bile can still flow into the intestines, aiding in digestion.
The duration of the Whipple procedure can vary significantly, typically ranging between four to six hours. The length of the surgery depends on several factors, including whether an open or minimally invasive technique is used and the complexity of the patient's condition.
Performing the Whipple procedure requires a high level of expertise and experience. Surgeons who specialize in this type of surgery are often trained in both general and gastrointestinal surgery. It's crucial to choose a healthcare provider with a proven track record of success in performing the Whipple procedure, as the surgery's complexity demands precise skill and care.
In conclusion, the Whipple procedure is a highly intricate surgery with the potential to offer hope to those battling pancreatic cancer. Whether through traditional open surgery or utilizing minimally invasive techniques, the expertise of the surgical team plays a vital role in the patient's recovery and outcomes. Understanding the process, from the organs involved to the reconstructive efforts post-removal, can help patients and their families prepare for what to expect during this challenging journey.
Remember to consult healthcare professionals for personalized advice and treatment options.

The Whipple procedure, also known as pancreaticoduodenectomy, is a complex and intricate surgery often used in the treatment of pancreatic cancer. As with any major surgical operation, it comes with its share of potential risks and complications, which are important for patients to consider before undergoing the procedure.
One of the most common complications following the Whipple procedure is postoperative infection. Infections can occur at the site of the surgery or in the abdominal cavity, potentially leading to more severe health issues if not treated promptly. Healthcare teams are vigilant in monitoring for signs of infection and are equipped to manage them should they arise.
Bleeding is another concern that can present either during or after the surgery. In rare cases, excessive bleeding may require additional operations to control. Advancements in surgical methods continue to improve ways to minimize this risk, ensuring a safer operation for the patient.
Additionally, the Whipple procedure can lead to issues related to digestion. Since this surgery involves the removal of part of the pancreas along with parts of the stomach, small intestine, and other nearby organs, patients may experience changes in their digestive process. Issues such as delayed gastric emptying where food remains in the stomach for longer than usual, or malabsorption, where the body has difficulty absorbing nutrients from food, can occur. Patients often work closely with dietitians to manage these changes, incorporating foods that are easier to digest and ensuring they receive the necessary nutrients.
It's also worth mentioning the potential for long-term diabetes management post-surgery due to changes in insulin production. This necessitates a careful and coordinated approach to diet and, in some cases, medication.
The decision to undergo the Whipple procedure is significant and requires a thorough discussion of these potential risks and complications with a healthcare provider. It's important to weigh these factors carefully against the potential benefits of treating cancer.
Despite these risks, for many individuals facing pancreatic cancer, the Whipple procedure offers a chance for treatment and potentially increased life expectancy. Each patient's situation is unique, making personalized medical advice crucial.
The Whipple procedure, a significant surgical operation primarily aimed at treating pancreatic cancer, entails a comprehensive recovery process. Understanding this journey is crucial for patients and their families as they navigate through post-operative life.
Typically, the hospital stay after a Whipple procedure can range anywhere from one to two weeks. This period allows healthcare providers to closely monitor the patient's condition, manage pain, and ensure that the digestive system is functioning properly before the transition to home recovery.
Once home, the recovery timeline can vary significantly among individuals, but generally, patients can expect a recovery period of about six to eight weeks. During this time, activities are gradually resumed, guided by the body's tolerance and the advice of the medical team.
Pain management is a critical component of the recovery process. Patients are usually provided with pain relief medications. Additionally, techniques such as relaxation exercises can also help manage discomfort.
Diet plays a pivotal role in recovery after the Whipple procedure. Initially, the diet is liquid-based, gradually moving towards more solid foods as tolerated. It is vital to consume foods that are easy on the digestive system. Recommendable options include vegetarian soups, smoothies, and eventually, whole foods like fruits and vegetables. Keeping hydrated and following a nutrient-rich, vegetarian diet aids in healing and energy replenishment.
Adhering to scheduled follow-up appointments post-surgery cannot be overstated. These appointments allow the surgical team to monitor the patient's progress, manage any arising complications, and adjust treatment plans as necessary. Regular follow-ups serve as a cornerstone for successful long-term recovery and health maintenance after the Whipple procedure.
In summary, recovery from the Whipple procedure is a gradual process that requires patience, strict adherence to medical advice, and lifestyle adjustments. With proper care, diet, and medical follow-up, patients can navigate their recovery journey effectively, aiming for a return to normalcy and vibrant health.
Undergoing the Whipple Procedure for Cancer is a significant life event that marks the beginning of a new chapter for many patients. This major surgery typically aims to address pancreatic cancer but may also be performed for other reasons. While it's a complex procedure, the advancements in medical science have improved long-term survival rates and quality of life for many individuals. Here, we delve into the critical aspects of life post-surgery, including lifestyle changes, dietary adjustments, and stories of resilience that inspire hope and encouragement.
After the Whipple Procedure, patients often need to make significant lifestyle changes. These might include increased rest periods to allow the body to heal and eventually, incorporating gentle exercises as recommended by healthcare providers. Ensuring adequate nutrition and hydration is also paramount, as is attending regular follow-up appointments to monitor recovery and health status.
Diet plays a crucial role in recovery and long-term health post-Whipple. Many individuals may find they need to adjust their eating habits to accommodate a more easily digestible diet. This often includes eating smaller, more frequent meals and opting for foods that are less taxing on the digestive system. Reintroducing high-antioxidant vegetables and fruits, whole grains, and protein from sources like lentils and tofu can provide necessary nutrients without overwhelming the digestive system. Consulting with a dietitian specialized in post-surgical nutrition can also offer personalized guidance and support.
The journey through cancer diagnosis, treatment, and recovery is deeply personal and varying. However, countless stories of resilience and recovery serve as beacons of hope for many. From individuals returning to their cherished activities to those finding new passions or ways to support others facing similar challenges, the spirit of human resilience shines through. Sharing these experiences can offer encouragement and a sense of camaraderie among those navigating life after the Whipple Procedure.
Survivors often emphasize the importance of a strong support network, including family, friends, and healthcare professionals, in their recovery. Emotional and psychological support through counseling or support groups can also be beneficial, helping individuals to process their experiences and embrace their new normal.
In conclusion, while the Whipple Procedure is a daunting prospect for many, the potential for improved quality of life and long-term survival is significant. Through making informed lifestyle and dietary adjustments, seeking support, and drawing inspiration from others' stories of resilience, life after surgery can be a journey of meaningful recovery and hope.
Undergoing a Whipple procedure for cancer can be a challenging journey, both emotionally and physically. It's a complex surgery that requires a comprehensive support system to help patients navigate through their recovery and beyond. Here, we'll explore a variety of resources aimed at providing patients with the care, support, and information they need during this critical time.
Connecting with others who have undergone similar experiences can be immensely comforting. Professional support groups offer a platform for sharing personal stories, tips, and encouragement. Organizations like the Pancreatic Cancer Action Network (PanCAN) provide access to patient-centered support groups that are facilitated by experienced professionals. These groups can be found both in-person and online, catering to patients varying needs and preferences.
The financial burden of cancer treatment can be overwhelming. Fortunately, there are organizations dedicated to easing this strain. The American Society of Clinical Oncology provides a comprehensive list of resources offering financial aid, including grants and assistance programs, to help cover the costs associated with the Whipple procedure and post-operative care. Additionally, the American Cancer Society can guide patients to financial resources and advice catered to their specific situation.
Nutrition plays a crucial role in recovery post-Whipple procedure. Engaging with a dietitian specialized in oncology can help patients establish a healthy eating plan that accommodates their new digestive system structure. Services offered by organizations like Zenonco.IO can connect patients with registered dietitian nutritionists skilled in oncology nutrition, ensuring patients receive tailored dietary advice to support their recovery.
The emotional toll of cancer treatment shouldn't be underestimated. Counseling services offered through cancer centers and organizations such as CancerCare provide access to licensed social workers and psychologists who specialize in cancer-related issues. These experts can offer strategies for coping with the emotional aspects of cancer recovery, including anxiety, depression, and stress management.
Embarking on the path to recovery after a Whipple procedure for cancer is a journey that patients shouldn't have to walk alone. Leveraging available resources, including support groups, financial aid, nutritional counseling, and emotional support services, can make a significant difference in the healing process. By staying informed and connected, patients can navigate their recovery with confidence and support.
The Whipple procedure, also known as pancreaticoduodenectomy, is a complex surgery performed to treat pancreatic cancer. Over recent years, significant advancements in research and technology have made this procedure safer and more effective for patients. This section delves into the latest developments and how they are improving outcomes for individuals undergoing this life-saving surgery.
One of the key advancements in the Whipple procedure is the use of minimally invasive surgery (MIS). MIS, including laparoscopic and robotic-assisted surgery, has been a game-changer. These technologies allow surgeons to operate with greater precision and flexibility. The benefits for patients are significant, including reduced post-operative pain, shorter hospital stays, and quicker recovery times.
Another significant advancement is the implementation of Enhanced Recovery After Surgery (ERAS) protocols. ERAS protocols are a set of standardized perioperative guidelines designed to reduce recovery time and improve outcomes. They focus on several aspects, including pain management, nutrition, and early mobilization. By adopting these protocols, patients undergoing the Whipple procedure experience improved post-operative recovery and a faster return to normal activities.
Precision medicine is also playing a pivotal role in refining the Whipple procedure. Tailoring treatment to the individual's genetic makeup allows for a more targeted approach to cancer care. Researchers are working on identifying genetic markers that can predict how patients will respond to surgery and other treatments, enabling a more personalized and effective treatment plan.
The use of 3D printing technology in surgical planning is another area of innovation. Surgeons can now create detailed 3D models of a patient's anatomy based on their MRI or CT scans. This allows for better preoperative planning and simulation of the surgery, which can lead to improved surgical outcomes and shorter operation times.
The Whipple procedure is challenging, but the ongoing research and technological advancements are promising for patients with pancreatic cancer. As the medical community continues to innovate, the prognosis and quality of life for patients undergoing this complex surgery will continue to improve.
Post-operative nutrition is crucial for recovery. While the focus is often on the surgical and technological aspects, proper nutrition cannot be overlooked. High-energy, protein-rich foods play a significant role in the healing process. Vegetarian options like lentils, beans, tofu, and quinoa are excellent sources of protein and essential nutrients conducive to recovery.
In the journey to conquer cancer, every patient's battle is unique. That's why personalized care is at the forefront of modern treatment approaches, recognizing the importance of tailoring both treatments and recovery plans to meet individual needs. This holds especially true for complex procedures like the Whipple procedure for cancer, a surgical treatment often used for pancreatic cancer.
Personalized care in cancer treatment involves a multidisciplinary team of specialists who work collaboratively to create a comprehensive treatment plan. This plan incorporates genetic testing, allowing doctors to understand the genetic makeup of the cancer and how it behaves. By identifying specific gene mutations, specialists can select the most effective treatments, potentially reducing the risk of side effects and improving outcomes.
Another critical component of personalized care is customized nutrition plans. Nutrition plays a crucial role in recovery and overall well-being during and after cancer treatment. Dietitians specializing in oncology nutrition develop tailored nutrition plans that not only support the body's healing process but also help manage the side effects of treatment. For individuals undergoing the Whipple procedure, a nutritious, vegetarian-based diet can be vital in supporting recovery, ensuring the body gets the necessary vitamins, minerals, and energy for healing.
Beyond medical and nutritional interventions, holistic care options are also an integral aspect of personalized care. Holistic care focuses on treating the whole person, not just the cancer. This can include physical therapy, psychological support, complementary therapies such as acupuncture, and lifestyle modifications. Each of these components is tailored to the patient's needs, preferences, and specific health situation, emphasizing a patient-centered approach to care.
Personalized care is a beacon of hope for many facing the daunting challenge of cancer. By focusing on the unique aspects of each patient's cancer and recovery journey, healthcare providers can offer more targeted, efficient, and compassionate care. This tailored approach not only enhances the effectiveness of treatments like the Whipple procedure but also supports patients' overall well-being, offering a more humane and supportive path through cancer treatment.
Undergoing a Whipple procedure for cancer can be a daunting prospect. Hearing from those who have walked this path before can offer invaluable insights and comfort. Here, we share real-life stories from patients who faced the challenges and triumphs of the Whipple procedure, aiming to shed light on the human side of this major surgical intervention.
Anna, a 52-year-old teacher, was diagnosed with pancreatic cancer. Facing a complex surgery, she was engulfed in fear and uncertainty. However, Anna's story is one of resilience. "The Whipple procedure was intense, and recovery was challenging. But, with a phenomenal medical team and the support of my family, I navigated through it. It's been a year, and I'm gradually reclaiming my life," she shares. Her experience underlines the importance of a strong support system and a positive outlook.
Michael, a 48-year-old software developer, underwent the Whipple procedure after being diagnosed with a tumor in his pancreas. "The journey was tough. Adjusting to life post-Whipple had its set of challenges, especially dietary changes. I switched to a vegetarian diet, incorporating foods that were easier to digest, like lentils, and soft-cooked vegetables," Michael recalls. His story highlights the dietary adjustments and lifestyle changes that are often necessary after the surgery.
Sara, 37, faced her cancer diagnosis with determination. Undergoing the Whipple procedure was a pivotal moment in her battle. "Post-surgery life was not easy. The recovery was long, and at times, I felt overwhelmed. However, every day I felt a little stronger," Sara reflects. Her experience emphasizes the emotional and physical rollercoaster that patients can expect and the gradual journey toward recovery.
These stories are a testament to the courage and resilience of individuals facing the Whipple procedure. They echo a common theme while the road to recovery may have its bumps, hope and support can guide patients through. If you or a loved one are preparing for this procedure, remember, you're not alone. Many have trodden this path and emerged stronger on the other side.