
Continent colostomy, also known as the Kock Pouch, represents a revolutionary approach in ostomy care, especially relevant for cancer patients enduring colorectal surgeries. Unlike traditional ostomy methods that require external bags, the Kock Pouch offers an internal solution, providing patients with a more manageable and discreet alternative. This innovation has dramatically improved the quality of life for countless individuals, granting them autonomy and control over their condition.
The concept of continent colostomy was developed in the 1960s by Dr. Nils Kock, marking a significant milestone in ostomy care. The principle behind this technique is to create an internal reservoir, which can be emptied at the patient's discretion. This is made possible by constructing a valve mechanism from the patient's intestines, thereby preventing the involuntary discharge of waste.
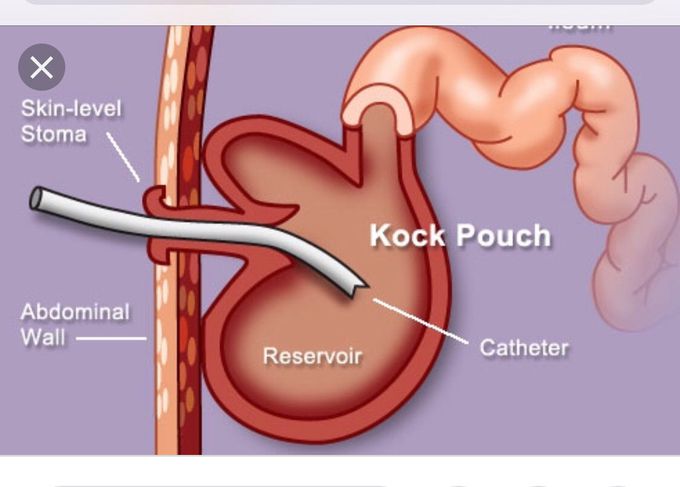
The surgical process involves fashioning a pouch from the patient's intestinal tissue. This internal pouch serves as a storage for fecal matter, which the patient can then expel using a catheter, thus eliminating the need for an external bag. The procedure is complex and requires a highly skilled surgical team, but the benefits it brings to the patient's life are profound.
Choosing a Kock Pouch over traditional ostomy methods offers several advantages, particularly for cancer patients who might already be grappling with the psychological and physical burdens of their condition. The most notable benefits include:
Adopting a Kock Pouch can be a liberating choice for cancer patients, allowing them to lead active, fulfilling lives despite their condition. However, patients need to consult with their healthcare provider to determine if this procedure is the best option for them, based on their specific medical history and lifestyle needs.
Post-surgery diet is crucial for Kock Pouch patients. A balanced, high-fiber diet is often recommended to facilitate the regular elimination of waste. Foods rich in fiber, such as fruits (e.g., bananas, and apples without skin), vegetables, and whole grains, are beneficial. However, patients should also keep hydrated and may need to adjust their diet based on their unique digestive responses.
In conclusion, the advent of the continent colostomy and the development of the Kock Pouch have opened new horizons for cancer patients, offering them a practical and discreet solution to manage their ostomy care. With the right support and medical advice, patients can indeed live life to the fullest, embracing the autonomy and dignity that everyone deserves.
Preparing for a Kock Pouch surgery requires an understanding of the preparatory steps, what the surgical process entails, and what to anticipate during recovery. This guide aims to simplify the journey for patients embarking on this significant healthcare journey, particularly in the realm of cancer care.
Before undergoing a Kock Pouch surgery, patients undergo a series of pre-surgical tests including blood work, imaging studies, and consultations to ensure they are suitable candidates for the procedure. During these consultations, it's crucial to discuss all medication and supplement use with healthcare providers to avoid any potential interactions.
Dietary adjustments are another essential aspect of preparation. In the weeks leading up to the surgery, a diet rich in fruits, vegetables, and whole grains is recommended to ensure the body is in optimal condition for recovery. Additionally, patients may be advised to follow a clear liquid diet 24-48 hours before the procedure to minimize complications.
Mental health considerations are also paramount. Many hospitals offer pre-surgery counseling to help patients manage anxiety and establish a support system for post-surgery recovery.
The Kock Pouch surgery involves creating an internal pouch, or reservoir, from the small intestine, which then is connected to the abdominal wall. The procedure typically requires a hospital stay of several days, during which pain management and monitoring for potential complications are priorities.
Post-surgery, patients are gradually reintroduced to solid foods and instructed on how to care for the stoma. Recovery times vary, but most individuals can resume normal activities within 6-8 weeks. It's essential to follow all provided guidelines and attend follow-up appointments to ensure the best outcome.
Potential complications, though rare, include pouchitis, stoma blockage, or difficulty in managing the stoma. However, with proper education and resources, these issues can be effectively managed or avoided.
In conclusion, preparing for Kock Pouch surgery requires careful planning and adherence to medical advice, but with the right preparation, patients can successfully navigate the surgical process and recovery. Embracing dietary adjustments and mental health considerations are key steps in ensuring a smooth transition before, during, and after the surgery.
Remember, it's crucial to maintain open communication with your healthcare team throughout the entire process. They are there to support you every step of the way, from the initial consultations through to your recovery and beyond.
Living with a Continent Colostomy, commonly known as a Kock Pouch, brings a new layer of complexity to daily life, especially for individuals who have undergone this procedure as part of their cancer treatment. However, with the right tips and practical advice, managing daily activities with a Kock Pouch can become manageable, allowing individuals to lead a fulfilling life. Below we explore dietary recommendations, hydration tips, physical activity guidance, and personal hygiene practices crucial for those with a Kock Pouch.
Maintaining a balanced, nutrient-rich diet is vital for individuals with a Kock Pouch. Emphasize whole, plant-based foods like fruits, vegetables, legumes, and whole grains. These foods not only provide essential nutrients but also help in maintaining regularity and minimizing digestion issues. It's advisable to introduce new foods gradually and monitor your body's response, as certain foods may cause gas or discomfort. Opt for vegetarian protein sources like lentils, beans, and tofu to enrich your diet.
Hydration is key to ensuring the smooth functioning of your Kock Pouch. Aim for at least eight glasses of water daily, and consider hydrating fruits and vegetables as additional sources of fluids. Beverages like herbal teas can also be soothing and beneficial. However, it's best to limit caffeine and alcohol intake as they can lead to dehydration.
Engaging in regular, moderate physical activity is important for overall health and well-being. Exercise can also aid in digestion and help prevent complications such as pouchitis. Start with low-impact activities like walking, swimming, or yoga, and gradually increase intensity based on comfort and endurance. Always consult your healthcare provider before starting a new exercise regimen.
Proper care and hygiene of your Kock Pouch are crucial to prevent infections and other complications. Regular, gentle cleaning of the stoma site with mild soap and water is essential. Draining the pouch multiple times a day, as recommended by your healthcare provider, will also keep it functioning well. Pay attention to signs of potential complications, such as unusual odors, leakage, or discomfort, and report these to your healthcare provider promptly.
In summary, while living with a Kock Pouch requires some adjustments, following these dietary, hydration, physical activity, and hygiene tips can significantly improve your quality of life. Always keep an open line of communication with your healthcare team for personalized advice and support.
For individuals diagnosed with cancer who have undergone a Continent Colostomy, popularly known as a Kock Pouch, adapting to their new reality involves navigating both physical and emotional landscapes. In this section, we delve into the personal stories of patients who have embraced life post-surgery and the insights from healthcare professionals to shed light on managing life with a Kock Pouch. Moreover, we'll uncover the psychological impact of this adjustment and the coping strategies that have proven beneficial.
Emma, a two-year post-operative Kock Pouch patient, shared, "Initially, it felt like my life was at a standstill. But, with time, understanding, and immense support from healthcare teams and patient communities, I learned to live fully again." Emma's experience highlights a common theme of resilience and acceptance in the face of adversity.
Dr. Alan Finch, a gastroenterologist specializing in post-colostomy care, emphasizes the importance of patient education and ongoing support. "The adaptation period varies for each patient. A multidisciplinary approach involving surgeons, gastroenterologists, and psychologists is crucial for a smoother transition," he comments.
Building a robust support system is paramount. Joining support groups, whether online or in-person, where experiences and tips are shared freely, can be incredibly empowering. Additionally, speaking with a psychologist skilled in chronic illness adjustment can provide further strategies for coping and emotional processing.
Regarding nutrition, adopting a balanced vegetarian diet is often recommended to ensure digestive comfort while meeting all dietary needs. Foods rich in fiber, such as lentils, beans, and a variety of fruits and vegetables, play a crucial role in maintaining a healthy gut environment.
The journey with a Kock Pouch is deeply personal and varies widely among individuals. However, the common thread among all stories is the capacity for adaptation and finding joy in life's new normal. Healthcare professionals stress the importance of patience, self-compassion, and reaching out for help when needed as key to the adaptation process.
In conclusion, living with a Kock Pouch after cancer is a significant adjustment that requires both psychological and physical adaptation. Yet through support, education, and shared experiences, individuals can navigate this journey with resilience, finding a new sense of normalcy and fulfillment.
The world of medicine is continuously evolving, with research and development delivering innovative solutions that significantly improve patient care and treatment outcomes. For individuals diagnosed with specific forms of cancer that necessitate a continent colostomy, such as colorectal cancer, advancements in surgical techniques and postoperative care have showcased remarkable progress, particularly in the implementation and improvement of the Kock Pouch.
Recent studies have delved into the effectiveness and patient outcomes associated with the Kock Pouch compared to its alternatives, such as the Barnett Continent Intestinal Reservoir (BCIR) and the ileoanal pouch. One key difference that has emerged from this research is the Kock Pouch's viability and preferred use in patients with specific cancer types, offering a more favorable prognosis and quality of life post-surgery.
In the realm of surgical innovations, minimally invasive approaches have been at the forefront, ensuring patients experience reduced post-operative discomfort, shorter hospital stays, and faster recovery times. For those undergoing the creation of a continent colostomy, such as the Kock Pouch, these advancements have been a game-changer.
The precise and less intrusive surgical methods now employed significantly lower the risk of postoperative complications, a common concern among patients. Enhanced screening and preparatory procedures further ensure that candidates for the Kock Pouch and other similar options are more accurately assessed, leading to tailored surgical plans that better meet individual patient needs.
Looking ahead, the future appears promising for those requiring a continent colostomy. Ongoing research is not only focused on refining surgical techniques but also on exploring novel materials and methods to further enhance the comfort and functionality of continent colostomy options.
Scientists are also investigating the potential of regenerative medicine and stem cell therapy as a means to even more effectively treat and potentially reverse damage to the digestive tract, which could revolutionize the approach to treating the underlying causes necessitating such surgeries.
When comparing the Kock Pouch to other continent colostomy options like the BCIR and the ileoanal pouch, several factors come into play. The Kock Pouch's design, aimed at preserving as much normal function as possible, offers a unique advantage for certain patient groups. Its valve mechanism designed to prevent leakage, for instance, presents a significant improvement in the quality of life for patients.
Each continent's colostomy option has its own set of advantages and considerations. The BCIR, for example, boasts an external stoma that can be easily concealed, while the ileoanal pouch does not require an external appliance at all. However, the choice between these options often boils down to the individual's condition, lifestyle, and the specific type of cancer involved.
Patients and their healthcare professionals must engage in thorough discussions regarding these options, taking into account the latest research and advancements in the field. Making an informed decision can lead to significantly improved outcomes and a better quality of life post-surgery.

Living with a Kock Pouch, or Continent Colostomy, following cancer treatment requires ongoing care and support. Patients and their families must access comprehensive healthcare services, understand insurance considerations, and find community support to ensure a high quality of life post-surgery. This segment is dedicated to providing essential information and answering frequently asked questions to make navigating these aspects simpler.
After undergoing surgery for a Continent Colostomy, patients will need regular check-ups to monitor their health and manage their Kock Pouch. It's crucial to find healthcare providers familiar with this specific type of colostomy. Patients can start by consulting with their surgical team or oncologist for recommendations. Additionally, many hospitals and cancer centers have specialized departments or coordinators who can assist in connecting patients with experienced gastroenterologists or colostomy nurses.
Make use of online directories and forums, such as the American Society of Colon and Rectal Surgeons (FASCRS) website, to find specialized care providers in your area.
Understanding your insurance coverage is key to managing the financial aspects of post-surgery care. It's advisable to contact your insurance provider to clarify what services and supplies are covered under your plan, especially since certain items specifically for Kock Pouch management may not be part of standard coverage. If you encounter challenges with coverage, patient advocacy organizations may offer guidance and assistance in appealing decisions or finding alternative funding options.
Remember, every patient's experience with a Kock Pouch is unique. Accessing the right resources and support is crucial to navigating the journey successfully. If you have more questions, don't hesitate to reach out to your healthcare provider or a support group for more personalized advice.